Chapter 3: Diagnosis of Obstructive Sleep Apnea (OSA).
Introduction
Did you know that many people are not aware of their sleep apnea’s symptoms and do not get diagnosed?
10 million Americans are unaware they suffer from the condition.
Fortunately, during the last decade, certain things have changed. A better knowledge of symptoms and clinical consequences have led to better screening methods.
But you should also be proactive.
There are many signs of sleep apnea.
Maybe you suffer from poor quality sleep, and your bed partner complains about your regular snoring.
Perhaps you:
- make choking sounds at night,
- suffer from restlessness during your sleep,
- frequently urinate during the night,
- and feel drowsy during daytime hours.
Or, possibly, you:
- feel tired,
- have headaches when you wake up,
- struggle to concentrate during the day,
- and suffer from sudden mood swings.
If you do, then take these symptoms seriously, and talk to your treating physician.
You may then have to see a sleep specialist for more in-depth exams.
That is right.
The diagnosis of sleep apnea requires specialized examinations.
Doctors use clinical symptoms, medical and family histories, and questionnaires.
You should inform your doctor if anyone in your family has had symptoms of this disorder or suffers from sleep apnea.
Diagnosis is not straightforward, and it will not happen during your first visit.
Let’s take a look at each step in detail.
Diagnosis of sleep apnea in children
If you have a child, then the diagnosis is simpler than in adults.
Why?
Because 80% of the time it is due to large tonsils.
So, what will your child’s doctor check first during the physical exam?
If you guessed the throat, then you guessed correctly.
The doctor will also check your child’s sleep history.
That is what he will usually begin with.
A physical exam and medical history may be enough to diagnose sleep apnea in young patients.
Medical history includes information about a person’s health such as:
- allergies,
- medications,
- surgeries,
- diet, etc.
In this case, it will be more focused on identifying symptoms related to sleep apnea, such as:
- sleepiness during the day,
- irritability,
- choking at night, etc.
As the parent, you should inform the doctor about your child’s signs and symptoms.
But what about adults? ….. Just continue reading. 😉
First steps to diagnose sleep apnea in adults: sleep history and physical exam
The first step consists of a routine exam.
Your doctor will begin by checking your sleep history.
That is about how you sleep, but also how you function at night.
He will ask if you:
- snore,
- suffer from daytime sleepiness.

He will also consider factors that increase your risk of suffering from OSA:
- obesity,
- retrognancy, that is your upper jaw (maxilla), or lower jaw do not occlude well because one of them is more posterior than it should;
- hypertension.
If your doctor’s findings are positive for this initial OSA screen, then it means you suffer from OSA, right?
Not quite, patience you must have, my young padawan.
What it means is that you are more likely to have OSA. In other words, you are at risk of suffering from OSA.
You will thus become a candidate for a more comprehensive sleep history and physical examination.
Curious to discover what these are, aren’t you? If so, then jump onto the next section.
More in-depths exams to diagnose sleep apnea
So, what do a more comprehensive sleep history and physical examination include?
Many more things that your doctor will check, namely:
- How often you snore, gasp, choke. Since you will likely not be aware of these, you will need help from your bed partner or a family member.
- Excessive sleepiness that cannot be explained by other reasons.
- Decreased libido.
- Non-refreshing sleep.
- Total sleep amount.
- Measurement of sleepiness severity by the Epworth Sleepiness Scale (see the below section for explanations about this test).
- Decreases in memory and concentration (cognitive functions).
- Sleep fragmentation/maintenance insomnia.
- Frequent urination at night (nocturia).
- Morning headaches.
- …
Also, your doctor should check conditions that may result from OSA such as:
- Hypertension.
- Stroke.
- Myocardial infarction.
- Decreased daytime alertness.
- Motor vehicle accidents.
- …
But there will also be an in-depth physical examination.
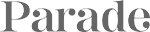
Your physician will look for the presence of extra or large tissues in your mouth, throat, and nose.
These include:
- enlarged soft palate, which is the roof of your mouth in the back of your throat,
- enlarged/elongated uvula,
- enlarged tonsils,
- large turbinates.
Besides signs of occlusion of the upper airway, he will also pay close attention to:
- obesity,
- increased neck circumference (> 17 inches in men, > 16 inches in women),
- deviated nasal septum, nasal polyps, …
- high arched/narrow palate
- …
See also: Are you at risk of developing sleep apnea? What are the risk factors for sleep apnea?
Depending on the results, you may be more or less at risk of suffering from OSA.
If you belong to the second group (less at risk), the timing for further testing will depend on the level of risk and symptoms or daytime impairment.
Otherwise, your testing will be expedited (because you are more at risk).
You will then have to undergo one of two tests that can confirm whether you are indeed an OSA patient.
But before delving into these two exams, let’s briefly touch upon the Epworth Sleepiness Scale that we mentioned above.
Diagnosis of sleep apnea and the Epworth Sleepiness Scale
At first glance, it sounds complicated.
But it is actually quite simple.
The Epworth Sleepiness Scale is a questionnaire aimed at measuring your chance of dozing off during the day.

Depending on the result, it may justify seeing a doctor, and going through more in-depth exams to assess whether you really have sleep apnea.
Beware though! … it is not a screening test for sleep apnea.
The Epworth scale only quantifies subjective somnolence irrespective of the presence or otherwise of a sleep disorder.
It assesses your level of sleepiness and amount of your quality sleep.
How does it work?
It calculates a score based on your “chance of dozing” in different situations such as when talking to someone or reading a book, etc.
Your “chance of dozing” can be slight, moderate, or high.
The higher the score, the lower the quality sleep you are getting, and the more tired you are.
Here below are some of the situations built into the Epworth Sleepiness Scale:
- Sitting and reading a document.
- Watching TV or at the movie theatre.
- Sitting inactive in a public place (e.g., a theater, conference, waiting room, meeting, lecture)
- As a passenger in a car or during public transport (train, bus, plane, underground) for an hour without a break.
- Lying down to rest and relaxing in the afternoon when circumstances permit.
- While sitting, during a conversation with someone close (also on the telephone).
- Comfortably sitting after a meal without alcohol.
- In a car, while stopped for a few minutes in a traffic jam.
You will have to analyze each of the above contexts.
Then you will need to decide what your odds of dozing are. These can be grouped as follows:
- 0: no chance of dozing.
- 1: dozing is possible but unlikely.
- 2: the probability of dozing is moderate.
- 3: it happens regularly, the likelihood of dozing is high.
What happens if your score is 6 or below?
Then you will be under the population average, which is 7 or 8.
If instead, it is 9 or more, then you have a problem, and should look for help.
This score is a strong indicator that you are likely suffering from OSA.
But to diagnose it with certainty, and to assess how severe the disease is, you need more than this.
In fact, your doctor needs to record:
- the number of shallow breaths (hypopneas);
- or breathing pauses.
You will be diagnosed with:
- light sleep apnea when you have 5-15 events/hour;
- moderate sleep apnea when 15-30 events/hours are recorded;
- severe sleep apnea, if you show 30 events/hour or more.
But how do you measure and capture all this information?
Through sleep studies which measure the quality of your sleep and how your body reacts to sleep problems.
Two methods are currently accepted standard of practice5 to diagnose your sleep apnea.
This is because of their accuracy.
The approved methods are:
- in-laboratory PSG;
- or home testing with portable monitors (PM).
Poly … what?
Jump to the next section to find out
What is a polysomnographic test?
It is a clumsy word for the most common sleep study.
This exam assesses if and which sleep disorder you suffer from.
Because there are many sleep disorders and OSA is just one of them, for instance:
- Sleep apnea,
- periodic limb movement disorder,
- REM behavior disorder,
- narcolepsy,
- …
In the USA, the test usually takes place in a sleep center (within a hospital or elsewhere).
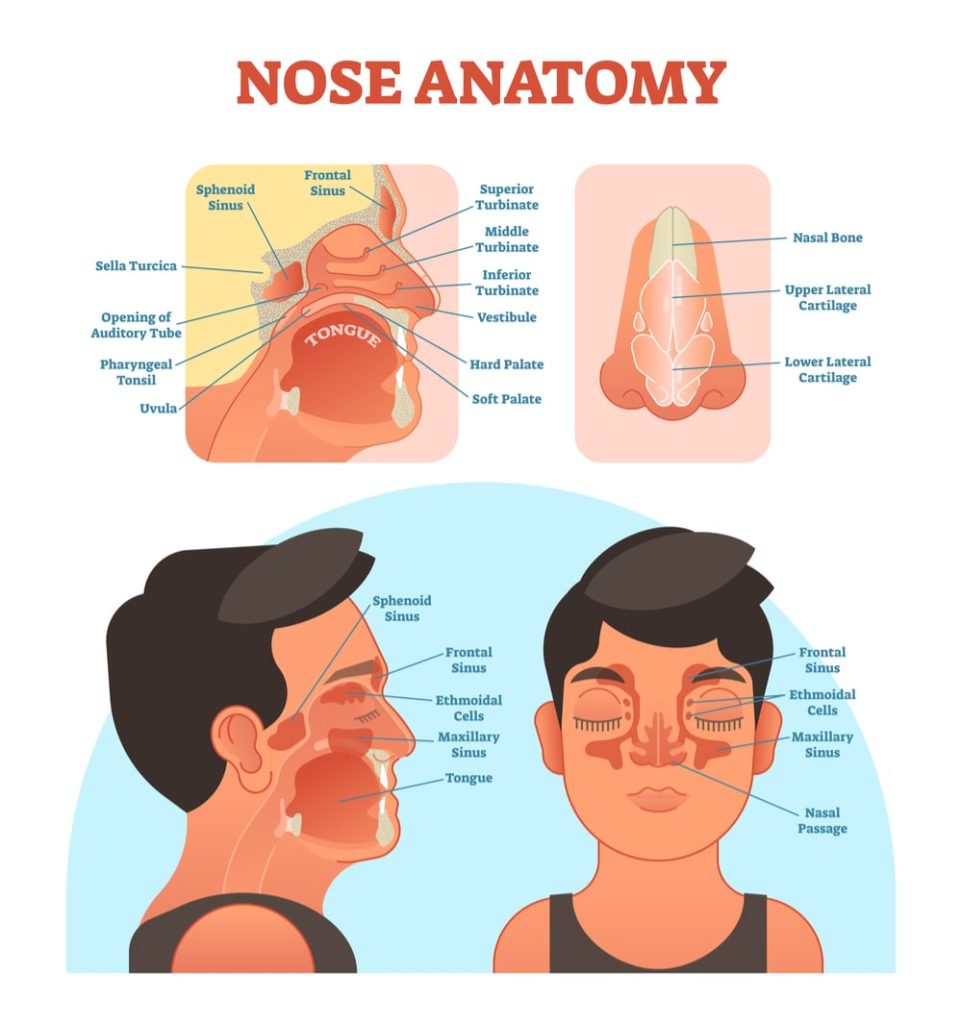
After your arrival, you will have to lie down and several wires will be connected to you.
But don’t worry!
The test is painless and takes place throughout your night sleep.
Trained staff will monitor you during this time while:
- your scalp,
- chest,
- limbs,
- and one finger,
will be attached to a bewilderment of wires and sensors.
But what exactly will they measure?
Your sleep specialist, or sleep technician, will capture numerous pieces of information, namely:
- airflow through your nostrils and mouth by means of air-pressure gauges;
- snoring;
- oxygen levels;
- breathing irregularities (mainly apneas and hypopneas);
- upper abdominal wall movement and chest wall movement. This will allow the doctor to see whether you are making an effort to breathe;
- blood pressure;
- cardiac rhythm abnormalities, that is if your heart beats too fast or too slowly;
- sudden shifts in brain activity (called arousals). They show sleep interruption due to your need to resume breathing. They may result from many factors, including:
- breathing abnormalities,
- leg movements,
- environmental noises, etc.;
- leg movements;
- eye movements.
The constant presence of a trained individual will ensure that:
- you follow the treatment,
- and that the instruments and probes can capture all the information required.
A qualified physician should review and interpret the data collected during your sleep study.
But what will be the critical information that will enable your sleep specialist to decide if you suffer from OSA?
Stay with us and read on.
When will PSG testing confirm that you suffer from OSA?
So, now we want to understand how a doctor can decide whether you suffer from OSA or not.
Which type of PSG measurement is critical?
The essential information is:
- the number of obstructive events (apneas, hypopneas + respiratory event related awakenings) is > 15 events/hour;
- or the number is > 5/hour, but you also show evidence of
- unintentional sleep episodes during wakefulness,
- daytime sleepiness,
- unrefreshing sleep,
- fatigue,
- insomnia,
- waking up breath holding, gasping, or choking,
- or the bed partner describing:
- loud snoring,
- breathing interruptions,
- or both,
- occurring during the patient’s sleep.
OSA, CPAP, and polysomnographic testing
After a PSG test, your sleep technician will be able to find out if you have OSA and decide your treatment (if needed).
If after a few hours of PSG testing, he thinks you suffer from OSA and that you need CPAP (check the following chapter Continuous positive air pressure), he may do a titration study.
A titra… what?
It is more straightforward than it sounds.
CPAP is the most frequently used treatment for sleep apnea. It handles moderate air pressures to keep your upper airway open during sleep.
Halfway through the night, your sleep technician may hook you up to a CPAP machine.
It is a way to take advantage of the fact that you are already connected to all sorts of sensors, to proceed with further testing.
The technician will spend the rest on the night gathering data to identify the best air pressure levels, possibly the optimal type of mask needed, etc.
You will be able to fall asleep comfortably because he will start at a low level and then gradually increase the air pressure.
Most CPAP machines come with a timed pressure “ramp” setting. Such a feature allows increasing air pressure up to the optimal level gradually.
What we described above is also referred to as a split-night sleep study:
- the first part of the night helps determine whether you suffer from OSA, and how severe it is,
- the second part is instead used to assess the best air flow from the CPAP machine.
Killing two birds with one stone!

A titration study is also used for sleep-related breathing disorders like:
- central sleep apnea,
- hypoventilation,
- and hypoxemia.
Let’s now look at portable monitors.
When to use home testing for OSA with portable monitors (PM)
Did you know that your sleep specialist may recommend the use of a home portable device for the exam?
Let’s first address the elephant in the room: can you always use a home portable device?
Because that would be an important time saver, wouldn’t it? (no need to go and sleep over in a center).
When can you not use it?
Okay, that is many questions.
Let’s check what guidelines say.
According to these you can use PMs to assess whether you suffer from OSA as part of a comprehensive sleep evaluation.
But this is only in patients with:
- high probability of moderate to severe OSA,
- and without other major associated diseases such as:
- moderate to severe pulmonary disease,
- neuromuscular disease,
- congestive heart failure,
- or those suspected of having a co-occurring sleep disorder.
The above notwithstanding, in some cases, PM testing may be the only solution for you.
When does this happen?
When you cannot be moved, such as when you are seriously ill, and in-laboratory PSG will not be a possibility.
Portable monitors will be effective at testing for OSA if they at least record:
- airflow (as you breathe);
- respiratory efforts like chest movements;
- blood oxygenation;
- your heart rate.
But that is not all…
According to the National Center for Biotechnology Information the same types of biosensors used for in-laboratory PSG should be used.
The results from your PM test should be assessed by a sleep specialist. For instance, he will verify whether you are making efforts to breathe etc.
In order to decide whether you suffer from OSA, he will need to do a comprehensive sleep evaluation and use the PM results.
The whole process may a take a few days or longer, after which he will contact you to discuss the conclusions.
But, but, but, … when compared to PSG testing …
… results from PM testing may underestimate the severity of apnea and hypopnea events.
This is important to know.
How may that affect you?
Well, if you have:
- a high pretest probability of suffering from OSA,
- and your PM exam is not enough to diagnose your OSA,
then your sleep apnea specialist will request an in-laboratory PSG.
In other words, he will use a more thorough exam as a way to check the validity of the PM results.
Good data means better decisions!
Your sleep specialist may also request further in-laboratory PSG testing if the PM device did not collect enough data.
How does home testing for OSA with portable monitors (PM) work?
I guess the advantage of home testing for OSA is clear.
Is it not?
If not, let me explain …
PM testing is very convenient since you will stay in the comfortable setting of your home.
You will also sleep while the instrument collects data.
The equipment will be delivered to your home, or you will have to go pick it up at your sleep specialist’s office.
Most of the times you will set up the instrument yourself, that is, after appropriate training by a technician.
Different PM devices come with various sensors and may differ slightly in what they measure.
You should make sure to ask the technician questions if you feel there is something you do not understand.
As for your daily routine, you should go to bed at your regular time but… don’t forget!
Before you lay down, you need to attach the sensors to different parts of your body as per instructions.
You will then have nothing else to do other than turn the machine on and go to sleep.
And that will be it.
In the morning, after detaching all the sensors, you will return the PM equipment (by mail or in person, to the sleep center).
Stay with us with you want to learn more about PSG and PM.
OSA, PSG or PM testing, surgery and dental appliances
If you suffer from OSA, what kinds of tests should you do before surgery?
According to guidelines, you should undergo:
- PSG or PM as part of a preoperative clinical exam, before you undergo upper airway surgery. This is true whether you suffer from snoring or OSA.
- PSG as part of a comprehensive sleep exam to assess whether you suffer from OSA before you undergo bariatric surgery.
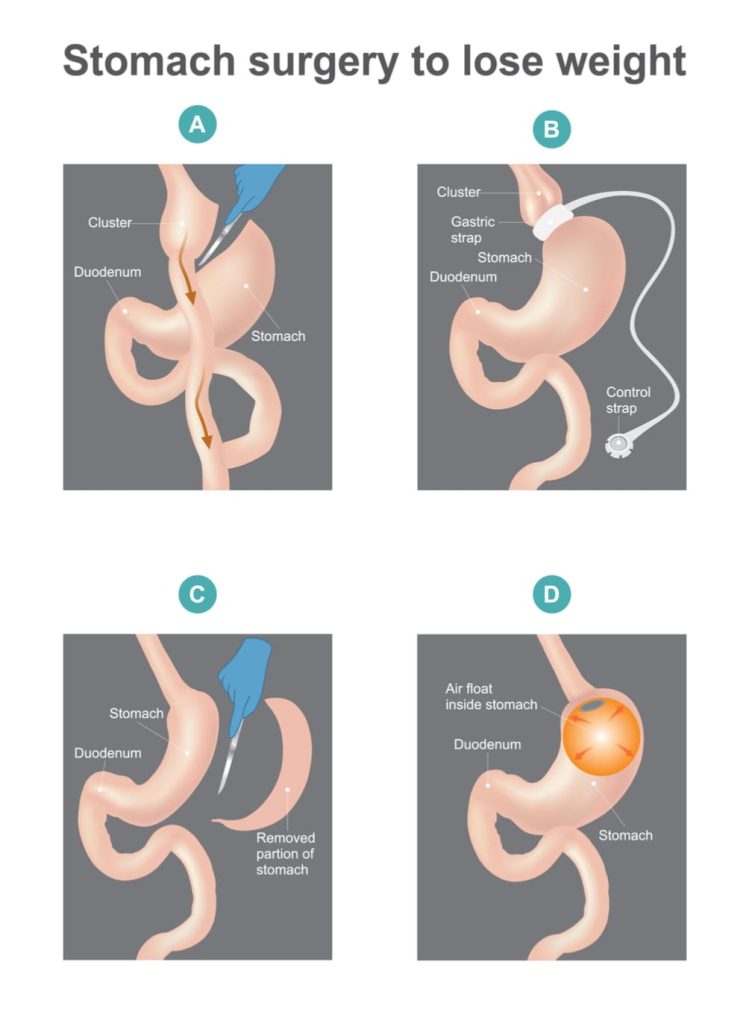
What about monitoring results after OSA treatment?
If you have used non-CPAP treatments such as:
- dental appliances,
- upper airway surgery,
- weight loss surgery,
then you may use testing at home (unattended by medical personnel).
Dental appliances and pulse oximetry
How does your dentist measure your improvements?
He uses a simpler approach than PSG, called pulse oximetry.
Also, it is low cost, and you can do it at home.
Although not as precise as PSG, it provides useful information.
Provided your dentist has been trained sufficiently, oximetry results are very useful.
He will gauge whether you have decreased the number of:
- complete cessations of breathing (apnea),
- and/or partial obstructions of breathing (hypopnea),
occurring per hour of sleep.
You can use both wrist as well as handheld readings obtained continuously over the night.
If results are not satisfactory, you will have to pursue treatment.
Otherwise, you will have to go back to your sleep specialist for a more in-depth exam.
This will confirm whether sleep apnea has indeed been resolved.
If resolved, then that’s good news, actually great news!
And that is because your dentist will no longer have to re-align your oral cavity. Only routine yearly visits are necessary after that.
Final Remarks
You have completed reading Chapter 3, congratulations!
Now it’s time to turn the treatment of OSA.
How?
By checking the following chapters:
- Chapter 4: Treating obstructive sleep apnea (OSA) with CPAP and dental appliances.
- Chapter 5: Treating Obstructive Sleep Apnea (OSA) with Surgery.
Though, also consider taking a look at the previous articles (if you have not already done so):
Chapter 2: Doctors Who Diagnose and Treat Obstructive Sleep Apnea.
Obstructive Sleep Apnea: The Definitive Guide for 2020.
Chapter 1: Obstructive Sleep Apnea (OSA) and its Health Effects.
SUTTON PLACE DENTAL ASSOCIATES ON THE WEB