Chapter 5: Treating Obstructive Sleep Apnea (OSA) with Surgery.
How can surgery treat sleep apnea?
Last but not least comes surgery.
Why last?
Because it is usually considered the third line of treatment after CPAP and dental appliances.
Can surgery be indicated earlier?
Yes, when your doctor identifies abnormal anatomical structures that:
- he can correct
- and which hinder device use.
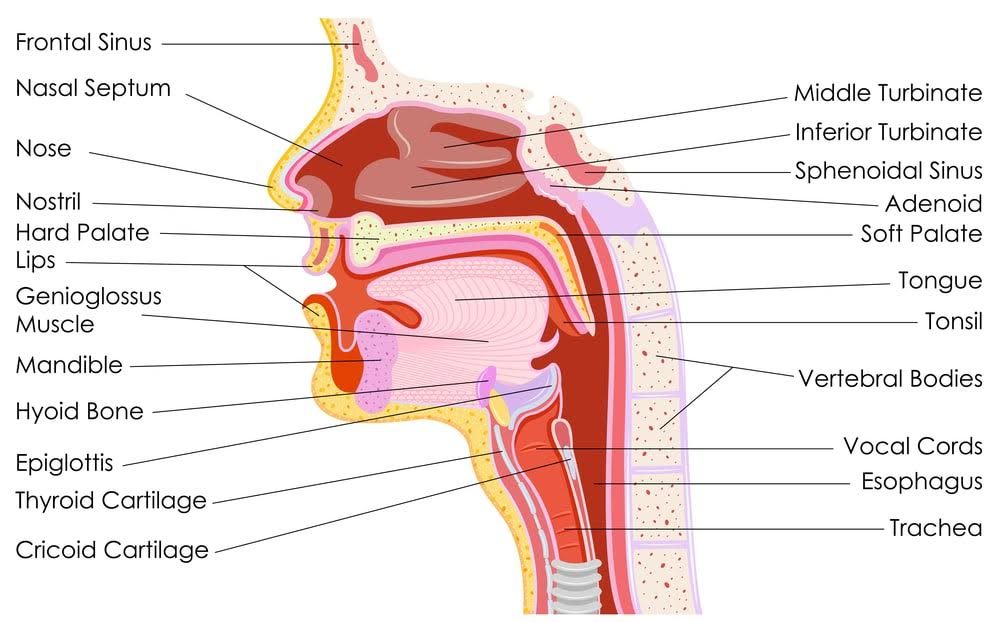
Now, you should know that there are many anatomical causes of sleep apnea.
Hence many surgical procedures exist to address each type of airway obstruction.
Each has its own risks and benefits.
Your surgeon’s choice will also depend on your age, whether you are overweight, obese or not.
Surgery can be targeted at soft tissues or/and skeletal structures. And your surgeon will choose the best procedure(s) for you.
Since surgery can improve your quality of life and survival …
… read on to discover the different techniques and success rates.
Nasal obstructions
F
Let’s start with the organ responsible for our sense of smell.
Surgery of the nasal cavity can:
- reduce inferior turbinates
- correct a deviated septum
- etc.
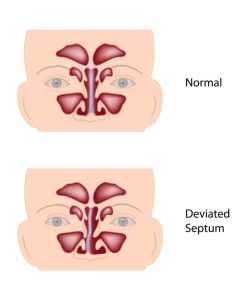
nasal septa
A deviated septum, as well as enlarged turbinates, tend to obstruct nasal airflow.
But is this surgery enough to help treat OSA?
Usually, not, you should not expect it to treat OSA on its own.
For this reason, correction of the nasal passage is often concurrent to that of oropharyngeal obstructions.
But, even on its own, it is far from useless.
Studies have shown that it is very beneficial since:
- it improves sleep quality,
- facilitates use of CPAP which in turn makes possible (a) more hours of treatment or/and (b) lower (CPAP) pressures.
Since we mentioned oropharyngeal obstructions, let’s dive deeper into the subject.
Oropharyngeal obstructions
These are redundant, flaccid and elongated tissues in the oropharynx.
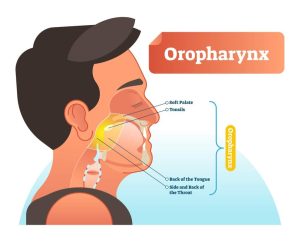
So you would expect surgery to focus on eliminating them, right?
Well, yes and no.
Pillar palatal implants, for instance, aim at local stiffening of the soft palate. They do not eliminate soft tissues to widen airway passages.
The procedure consists of:
- the insertion of thin, narrow, polyester implants in the soft palate (which is the roof of the mouth)
- with a modified syringe.
By reducing vibration and collapsibility, it can:
- treat mild OSA with mild-to-moderate effects
- reduce snoring with moderate effects.
But these implants are not the most frequently used surgical procedure for treating OSA in adults.
The prize instead goes to Uvulopalatopharyngoplasty (UPPP).
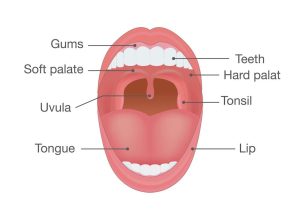
It is used to remove several soft tissues that may obstruct your airways at the back of the throat:
- Part, or all, of the uvula,
- parts of the soft palate and tissue at the sides of the throat,
- tonsils and adenoids, if still present.
UPPP’s results with OSA vary a lot depending on the size of the tonsils and the patient’s body mass index.
It can improve patients’ compliance with CPAP by lowering CPAP pressure requirements (see also Chapter 4: Treating obstructive sleep apnea (OSA) with CPAP and dental appliances).
Let’s now move to study surgical procedures of the tongue to treat OSA.
Surgeries of the tongue
Your surgeon can use several procedures to treat obstructions due to the tongue.
And guess what?
All in all, symptoms of daytime sleepiness and quality of life are generally improved with all tongue procedures.
But let’s understand how the tongue can obstruct the airways passage.
One possibility is that you can have more fat deposits at the back of your tongue. You will thus have a larger than normal base of tongue size.
You could also suffer from an abnormally large tongue. Your surgeon will thus try to reduce its size.
But how? Well, let’s see…
Midline glossectomy
This is the name of a procedure that he may use.
It consists of removing the central part of the tongue base (at the back of the tongue).
The success rate can vary between 25-83%.
Genioglossus muscle
Another approach involves your genioglossus muscle.
Genio… what?
This is the largest muscle of your tongue. It allows you to protrude it (or stick it out).
Surgery consists in moving its anchor point in the bone – the genio-tubercle – forward.
The result is less obstruction of the airways when sleeping as the tongue relaxes during sleep.
The success rate can vary from 39 to 78%.
Radiofrequency
Radiofrequency ablation is also used.
This makes use of radio waves which create a certain amount of controlled damage in your tongue.
The resulting scarred repair tissue will shrink the tongue slightly.
The likelihood of the tongue falling back during sleep will also decrease.
It will be successful at improving snoring.
As for your sleep apnea, the surgical success rate will be in the order of 36%
Hyoid suspension
Although it has a strange name, the hyoid is actually a little bone.
That’s right, just a little U-shaped bone, in the neck.

found at the Root of the Tongue
You can find it above Adam’s apple.
It is attached to several soft tissues and muscles in the throat and tongue.
It is free to move around which may lead to the collapse of the structures that attach to it during sleep.
This may, in turn, cause the airway to get blocked.
Your surgeon can suspend and advance it to increase space at the base of the tongue.
Results are variable, and it is performed as an adjunctive surgery for the treatment of OSA.
Tongue suspension techniques
As the name suggests, your tongue base is pulled forward or suspended to reduce obstruction (at its base).
How?
Your surgeon will pass nonabsorbent sutures through your tongue and attach them to the jaw bone using a screw.
The technique is minimally invasive and can be performed along with other techniques (or on its own).
The success rate is approximately 33%.
Let’s now look at a radical approach to treat your OSA: craniofacial surgery.
Craniofacial surgery
As you may have guessed already, this involves more complex surgical procedures.
Hence, it is usually the last phase of surgical treatment.
In some selected cases though, your surgeon may propose it as an initial approach. He can do this to avoid many surgeries.
It is also proposed as an initial option when your OSA is not the result of soft tissues abnormalities.
So what does craniofacial surgery consists in?
Different procedures which may include advancement:
- of the inferior part of the jawbone and hard palate,
- of the anterior jaw,
- of the facial skeleton which will pull your soft tissues forward.
The end result is the widening of the entire pharyngeal space or posterior airway space. This will ease your breathing.
What about the success rate?
With 43% positive results, the success rate is the highest among different surgical interventions.
Several studies have shown that it is equal in effectiveness to nasal CPAP.
It is now time to look at a completely different type of surgery, which no longer involves your head’s tissues and structures: bariatric surgery.
It can help you lose weight (and in turn treat your OSA). Hence its accelerated growth, especially after the introduction of minimally invasive techniques.
Weight Loss by Bariatric Surgery
Do you know how often OSA is present among very obese patients?
The answer is …almost half, that is 45%.
Pause for a moment, and let that sink in.
Studies have shown that even mild-to-moderate weight loss benefits overweight patient.
Very obese patients who have failed to lose weight via standard treatments like:
- low-calorie diet,
- behavioral changes,
- exercise and activity,
may be advised to undergo bariatric surgery.
Now, let’s see what the impact (of surgery) on OSA is.
Two authors report some interesting results:
- 101 patients who received bariatric surgery saw their AHI decreasing from 51 ± 4 (preoperatively) to 15 ± 2 (postoperatively).
And this without them receiving any other treatment. - OSA patients showed remission rates of 40% after bariatric surgery.
So, results are more than encouraging.
Last but not least, read on to discover how subsequent (staged) surgical interventions can treat your OSA.
Multi-level surgery and staged surgery
A quick question for you…
What percentage of patients suffer from OSA as a result of only one site obstructing the airways?
……. Only 25% whereas a vast 75% of patients have multi-level obstructions. So you are likely to have involvement of two or more of the following anatomical areas:
- soft palate,
- lateral pharyngeal walls,
- and tongue base.
If you suffer from many obstructions, single-site surgery will have a poor success rate.
Studies instead show that you can get success rates as high as 95% when different surgical approaches address many levels of obstruction.
Are surgical protocols all done in one event?
No, they are usually staged if there are many abnormalities present.
Your surgeon will do the less risky procedures first. Meaning the ones less prone to complications will be prioritized.
Some examples of combined surgeries include:
- Advancement of your genioglossal muscle along with Uvulopalatopharyngoplasty (UPPP). The former will enlarge the airway at the base of your tongue.
- An oropharyngeal procedure and a nasal procedure.
All you have been reading until now was valid for an adult population.
But what about children?
….Well, check the next section to find out what happens with little patients.
Children and sleep apnea surgery
If you have children, you should be wary that obstruction of the upper airways is not without its effects.
This is true even in small patients.
It can:
- Hinder the growth of their upper and lower jaws. This can, in turn, change their craniofacial structure which could worsen OSA once adults.
- Create behavioral problems such as hyperactivity.
- Lead to suboptimal school performance.
So if you could avoid all that, then it would be hugely important, right?
But how do doctors decide whether your child suffers from OSA?
The criteria for deciding are stricter than in adults.
Some experts go as far as saying that an AH> 1 is enough to diagnose your child with OSA.
Now, surgery to treat OSA in children is very different from an adult population:
- it consists mainly in removing the tonsils if they are too large and obstruct the airways. (It is one of the most common surgeries in the pediatric population).
- It is a first-line therapy unlike in adults, where CPAP or dental appliances are instead first-line (usually).
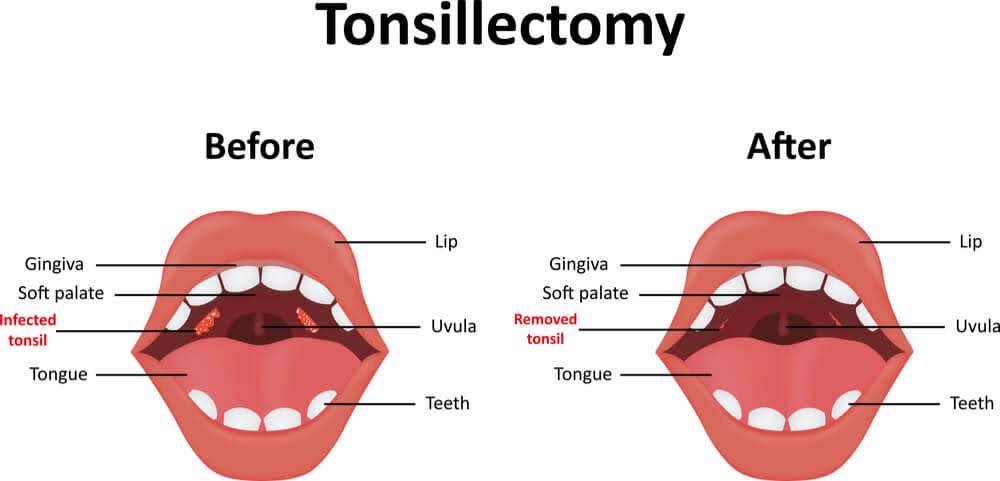
Removing the tonsils is curative in 80% of children suffering from OSA.
It is also worth noticing that tonsils tend to shrink as children grow.
So do not be surprised if your doctor suggests waiting some time before deciding for surgery.
That is all for pediatric patients.
Let’s briefly talk about results after surgery in the adult population, before we wrap up.
OSA results after surgery
So, by now you have probably understood that results can vary a lot from patient to patient.
Surgery is not the open-sesame to resolving OSA.
And this is because OSA has many different concomitant causes and factors.
These include varying patient characteristics such as the age or body mass.
Also, types of obstructions can be very different.
Though, surgery will still provide some important benefits for you:
- reduction of early mortality risk and cardiovascular risk
- improvement in “reaction time, quality of life, and motor vehicle crash risk”
But are results with OSA forever (like diamonds)?
The answer is awaiting you in the next section.
How long do results of OSA surgery last?
That is a good question.
Human muscles and tissues lose tonus as we get older. They become more collapsible.
Hence, the effectiveness of your surgery will likely decrease with time.
Also, we tend to become overweight as we become more mature 😊.
Now, weight gain seems to be one of the main factors making you more prone to losing the positive effects of the surgical treatment.
Thus, it is advisable that you regularly see your treating doctor to get a long-term follow-up.
This is actually independent of the treatment you have chosen.
If you have read until here, then you are almost an expert. Just one more section to go.
How well do Uvulopalatopharyngoplasty (UPPP), CPAP and weight loss treat OSA?
A study with 444 patients provided some interesting insights.
This group was made of patients with and without OSA.
Those with OSA were either treated with UPPP, weight loss, CPAP or not treated at all.
Guess what?
The untreated group had higher mortality than the group not suffering from OSA.
But those treated, irrespective of the treatment, had survival rates similar to the healthy group.
And that’s all folks! We hope you have enjoyed the article.
Final remarks
Congratulations!
You have made it!
You have now reached the stage of “all-knowing” about OSA 😊.
In case you are almost there but not quite, make sure you read some of the previous articles (chapters) of the definitive guide to sleep apnea:
(Chapter 5: Treating Obstructive Sleep Apnea (OSA) with Surgery.)
Obstructive Sleep Apnea: The Definitive Guide for 2020.
Chapter 1: Obstructive Sleep Apnea (OSA) and its Health Effects.
Chapter 2: Doctors Who Diagnose and Treat Obstructive Sleep Apnea.
Chapter 3: Diagnosis of Obstructive Sleep Apnea (OSA).
Chapter 4: Treating obstructive sleep apnea (OSA) with CPAP and dental appliances.
SUTTON PLACE DENTAL ASSOCIATES ON THE WEB