Chapter 1: Obstructive Sleep Apnea (OSA) and its Health Effects
Introduction
We all know that after a night of poor sleep we tend to be temperamental, moody, struggle to concentrate and feel fatigued.
But what about the consequences of prolonged lack of sleep on your health?
How is your health affected?
Unfortunately, the answer is short: sleep apnea hurts your health.
And what is worse is that you will often not be aware of the extent of the issues.
The development of sleep apnea is gradual.1
But, a study has shown that moderate-to-severe sleep apnea increased mortality significantly.2
So, if you suffer from sleep apnea syndrome your quality of life as well as your life expectancy will decrease significantly.
Some studies have investigated the impact of lack of sleep on different diseases.
If left untreated, sleep apnea may increase the risk of:3
- arterial hypertension,
- heart attack,
- stroke,
- heart failure,
- irregular heartbeat,
- diabetes type 2,
- obesity,
- depression,
- erectile dysfunction,
- loss of libido,
- concentration and memory loss,
- risk of motor vehicle collisions,
- work related accident,
- Alzheimer disease,
- …
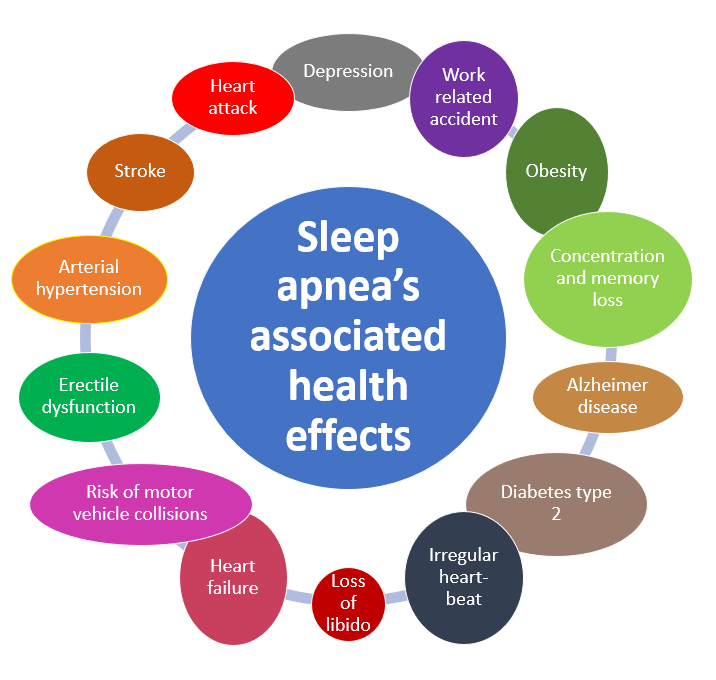
Let’s take a closer look at each of these effects, one by one.
Table of contents
- Introduction
- Are OSA and cardiovascular diseases related?
- How OSA influences cardiac health?
- Does OSA influence hypertension?
- Heart failure and OSA
- How are OSA and coronary heart disease related?
- Does OSA influence your risk of a stroke?
- Does OSA influence the potential for recovery after a stroke?
- Does OSA influence the risk of sudden cardiac death?
- Does OSA influence irregularity of heartbeat?
- How are OSA and diabetes 2 related?
- How are OSA, diabetes Type 2 and cardiovascular diseases related?
- Does OSA increase the chance of a motor vehicle accident?
- How many lives would be saved if apneic patients were treated with CPAP?
- OSA and work-related accidents
- How are OSA and insomnia related?
- OSA and erectile dysfunction (ED)
- How does OSA influence mood disorders?
- How does obesity influence OSA?
- How does OSA affect the risk of cancer?
- How does OSA affect you’re your mental capabilities (cognitive functions)?
- How are OSA and Alzheimer disease related?
- Final Remarks
Are OSA and cardiovascular diseases related?
What should you do if you see that your bed partner or a family member frequently stop breathing for short moments?
There are no doubts!
You need to encourage him (or her) to seek medical advice straight away.
And that is because OSA can lead to premature cardiovascular death.
Why?
Because, according to the American Heart Association (AHA), it is associated with:4
- high blood pressure,
- arrhythmia or irregular heartbeat,
- heart failure,
- coronary heart disease,
- and stroke.
Always according to the AHA, the evidence for a relationship between sleep apnea and high blood pressure is important.
And one should not forget that high blood pressure is a major risk factor for:
- coronary heart diseases
- and stroke.
Furthermore, the former is the leading cause of death in the USA. As for the latter, it is an important cause of disability and death.
Let’s try to understand better the relation between OSA and cardiovascular diseases.
How does OSA influence cardiac health?
If you have been diagnosed with OSA then you know that:
- your heart,
- your blood vessels (arteries, capillaries, veins),
- and your brain,
will be exposed to periods of lack of oxygen (hypoxia) many times throughout the night.
(Note: your blood vessels and heart make up your cardiovascular system).
At night you will experience a below normal (negative) intrathoracic pressure.
Why?
Because you will struggle to breathe. You will experience pauses in your breathing due to a blocked airway.
Each sudden micro-awakening will lead to an increase in the arterial pressure and cardiac rate. This will result in a lot of strain on your heart.5
Here is that way it works:
- as your brain detects oxygen levels’ drops,
- it will “tighten” the vessels to increase blood pressure,
- to improve the oxygen supply.
You now understand why OSA will increase your risk of developing cardiovascular diseases.
The mechanisms via which the whole process happens, are not entirely understood. But treating OSA has the potential to diminish such risk.6
Let’s now look at hypertension.
Does OSA influence hypertension?
Different studies have focused on the connection between OSA and blood pressure.
Patients with OSA are often also obese and have other co-existing diseases as well.
How does that pose a challenge?
Because you need to gauge which part of blood pressure increase is due to your:7
- OSA,
- obesity,
- or to an interaction between these.
But, authors believe that there is a strong association between OSA and hypertension.8
An estimated 50% of patients with hypertension suffer from concomitant OSA.9
You will thus be much more likely to present OSA if your blood pressure is high.
And if you are in doubt, think about this for a moment. If you suffer from hypertension, then the American Academy of Sleep Medicine (AASM) advises that you be evaluated for sleep apnea.
The AASM suggests contacting a board-certified sleep medicine physician for this.
Do you understand why?
It’s simple! They consider the clinical evidence showing an increase in OSA amongst patients with hypertension, to be overwhelming.10
Let’s now look at the link between OSA and hypertension.
The mechanism via which it probably affects your blood pressure is not entirely understood.
But, the drops in your blood oxygen levels during your nightly apneas probably play an essential role.
Your brain detects these drops via appropriate receptors. It will then signal your vessels to constrict (via the nervous system).
And constriction helps to increase blood flow to:
- the organs,
- the brain,
- and heart especially.
And that is easy to understand.
Unfortunately, often, your blood pressure will remain high also during daytime.
And this despite your breathing is back to normal.
That is more surprising, right?
This phenomenon is probably due to different mechanisms. These are triggered by the low oxygen levels you experience during your sleep.
Are you wondering if you need to treat your OSA to keep your hypertension under control? If so, then read does treatment with cpap continue to influence hypertension in osa patients
Let’s now delve into another specific cardiovascular disease… heart failure
Heart failure and OSA
But what exactly is heart failure?
Not exactly a minor issue, as you already know.
It is a condition in which the heart can’t pump enough blood to meet the body’s needs.
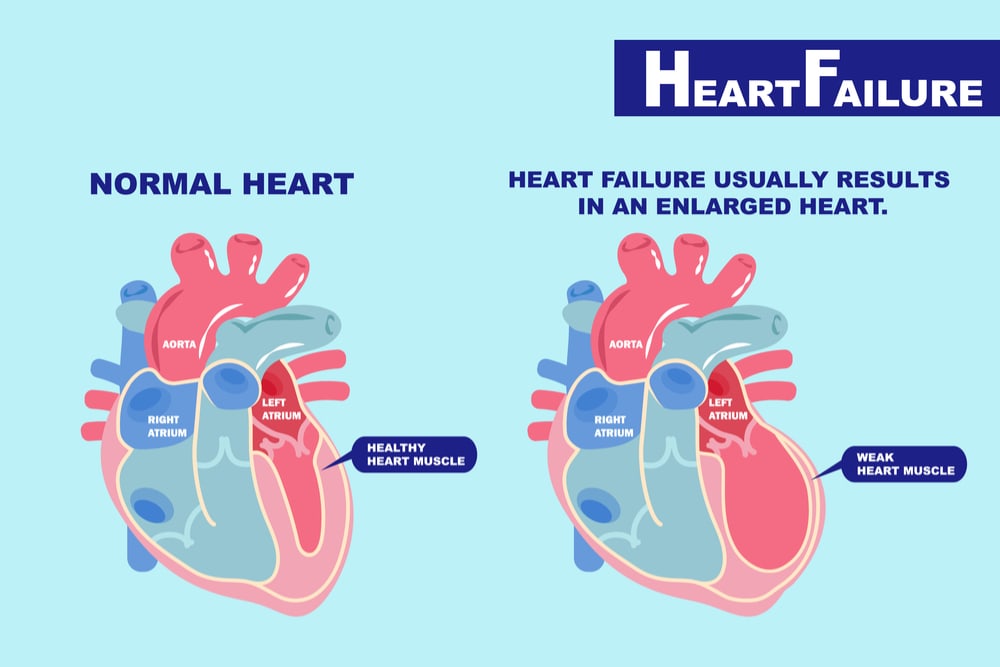
In some cases, not enough blood can fill the heart.
In other cases, the heart can’t pump blood to the rest of the body with enough force.
Some people have both problems.
The relation between OSA and heart failure is well understood … right?
Wrong!
Unfortunately, this patient population suffers from other diseases. Hence, understanding the relation is difficult.
But some things are known. For instance, studies in populations have shown that, if you have heart failure:11
- the chance of having OSA exceeds 50%,
- OSA can worsen the course of the disease increasing associated illnesses and mortality.12
Now, let’s talk about coronary heart disease and OSA.
How are OSA and coronary heart disease related?
You probably already know what coronary heart disease is.
But if it is a bit fuzzy, here is a refresher explanation.
It is a disease characterized by:
- a slow process that hardens and narrows the arteries, which provide oxygen-rich blood to your heart muscle,
- via the build-up of a waxy substance called plaque,
- which gradually reduces the diameter of these vessels.
Narrow coronary arteries can become blocked, and lead to heart attacks.
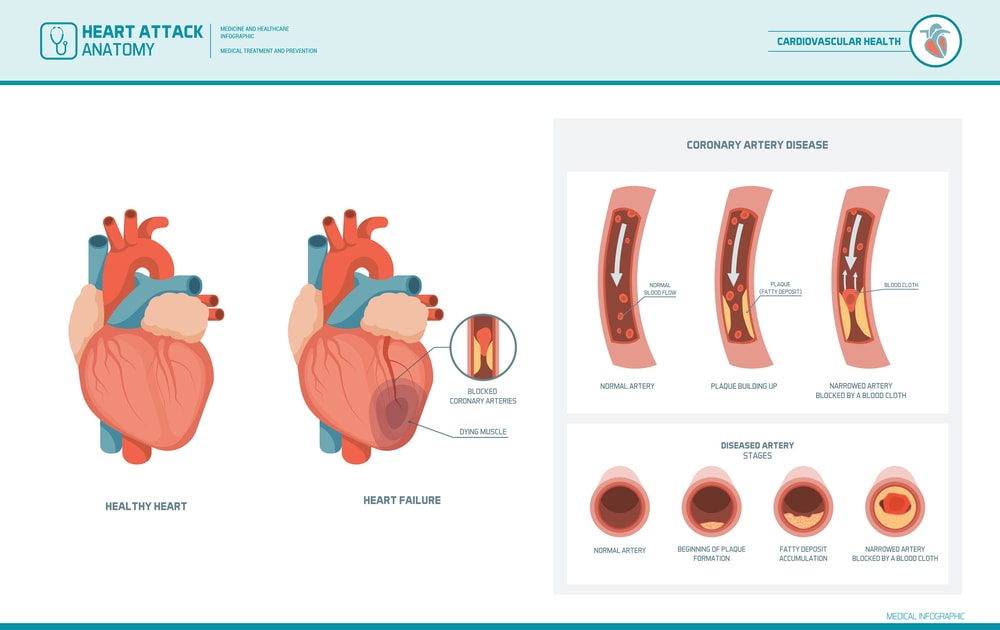
Studies (case-controlled) have shown that OSA was very frequent in patients with coronary heart disease.13 14
But, as if that were not bad enough, …
… patients treated with a stent for coronary heart disease had poorer results if they also had OSA.
This group of patients showed higher:15
- cardiac death,
- reinfarction,
- re-narrowing of coronary arteries after stent implantation,
than those without OSA.
So, should you seek treatment for your OSA, if you are suffering from coronary heart disease?
Check: …
… to discover the answer.
Let’s now learn about OSA and stroke.
Does OSA influence your risk of a stroke?
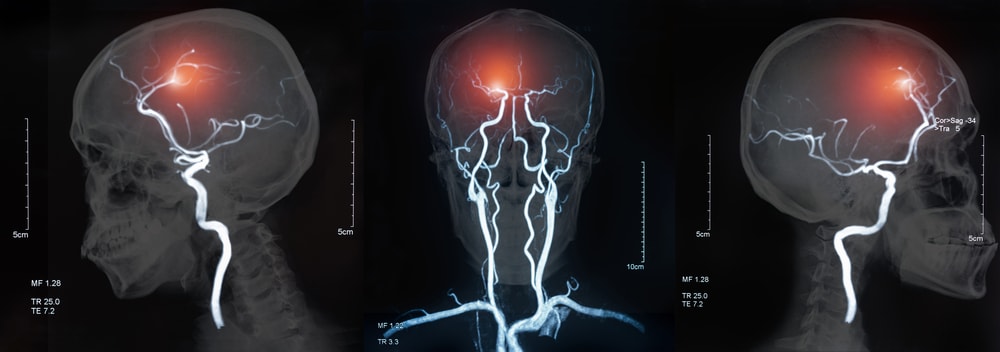
Given the , the relation between a stroke and OSA is well established (?)
Wait, it is not so simple.
It is still unclear how and if sleep apnea causes a stroke.
However, yes … unfortunately, sleep apnea does increase your risk of suffering from a stroke.
Large studies have shown that you will be more likely to suffer from a stroke in the future if you have sleep apnea.18
This is true even after discounting other factors that may increase your chances of having a stroke, like19:
- high blood pressure,
- smoking status,
- diabetes mellitus,
- high cholesterol,
- atrial fibrillation (irregular heartbeat).
Read on to discover how OSA affects your chance of recovery from a stroke.
Does OSA influence the potential for recovery after a stroke?
The answer is a resounding yes20, unfortunately.
OSA may in fact:
- Negatively affect the potential for recovery in stroke patients.
- Increase the length of time spent in a hospital and the risk of death.
And what about sudden cardiac arrest?
Next…
Does OSA influence the risk of sudden cardiac death?
Again, the answer is … yes21.
Irrespective of whether:
- You are obese or overweight,
- or suffer from other risk factors,
OSA increases the risk of a heart attack.
Interestingly, people with OSA have a peak in sudden death from cardiac causes during sleeping hours.22
But what is so special about that?
Well, it is exactly the opposite of the rest of the population:
- Here a heart attack happens mostly during the morning hours, after waking up.
- The lowest risk is during sleep (i.e., from midnight to 6 a.m.).
Finally, a study in a population of 10,701 adults who underwent showed worrying results. It showed that sudden cardiac death was much higher among severe OSA patients.
These were subjects who stopped breathing or had shallow breathing more than 20 times an hour during sleep.23
And now, last but not least among cardiovascular diseases, let’s look at irregular heartbeat and sleep apnea.
Does OSA influence irregularity of heartbeat?
Problems with the rhythm of your heart can be life-threatening.
And if you are apneic, how will that affect your heart’s behavior?
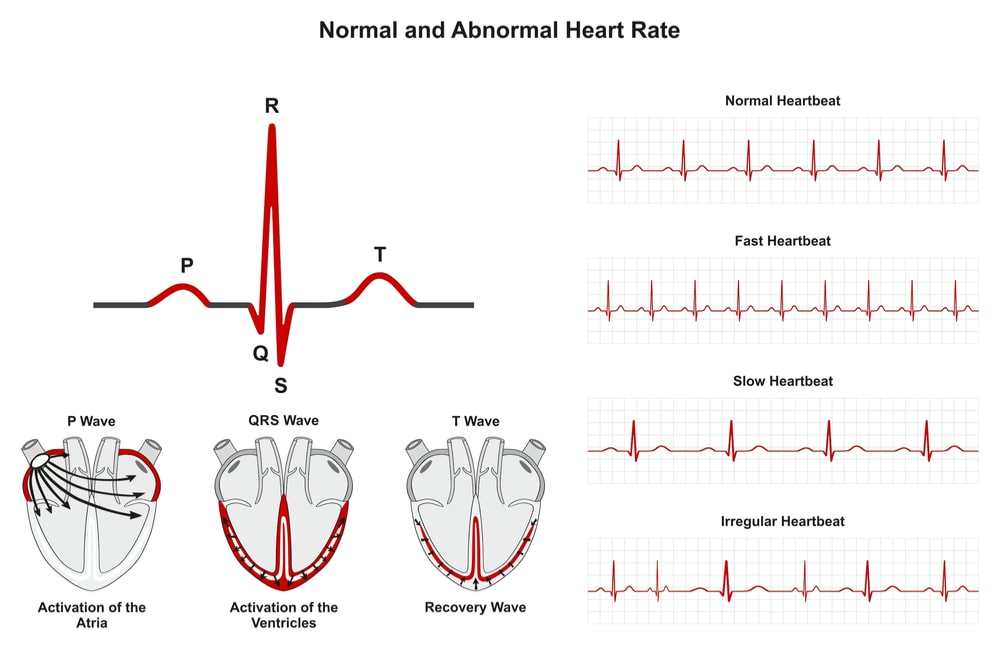
You have probably already guessed the answer.
If you suffer from OSA, then things get worse, and your risks of irregular heart behavior are higher.
You will be more likely to suffer from:
- An irregular heartbeat,
- and irregular traveling of electrical impulses through your heart (which cause it to beat).
This will be true for both:
- Atrial fibrillation (irregular heartbeat),
- and bradycardia (slow heart rate).
A study found that if you suffer from severe sleep-disordered breathing:
- you will have 2-4 more chances of suffering from complex arrhythmias,
- than if you don’t suffer from sleep-disordered breathing.
This was true after correcting (discounting) for other factors that could influence the observations such as24:
- age,
- sex,
- concomitant coronary heart disease …
And, unfortunately, these are not good news since:
- atrial fibrillation is a major risk factor for stroke,
- and ventricular tachycardia is a cause of sudden death.
Also, if you undergo cardiac ablation, you will have a 25% higher risk of having your atrial fibrillation return, if you also suffer from OSA.25
Now dear reader, given what we just read, it makes perfect sense to treat OSA, in case you were suffering from an irregular heartbeat.
Wouldn’t you agree?
Learn more by visiting: does treatment of obstructive sleep apnea reduce cardiac arrhythmias>
Let’s now move out of cardiovascular diseases and learn about OSA and diabetes.
How are OSA and diabetes 2 related?
Before answering that, here is a brief recap of the difference between diabetes Type 1, Type 2 and impaired glucose tolerance:
- in diabetes Type 1, your own immune system attacks your pancreas (autoimmune disease). As a result, it stops producing insulin.
- Instead, if you suffer from diabetes Type 2:
- your pancreas produces insulin to a certain extent;
- these amounts may not be enough for your needs, or your cells may not use them efficiently (have become resistant).
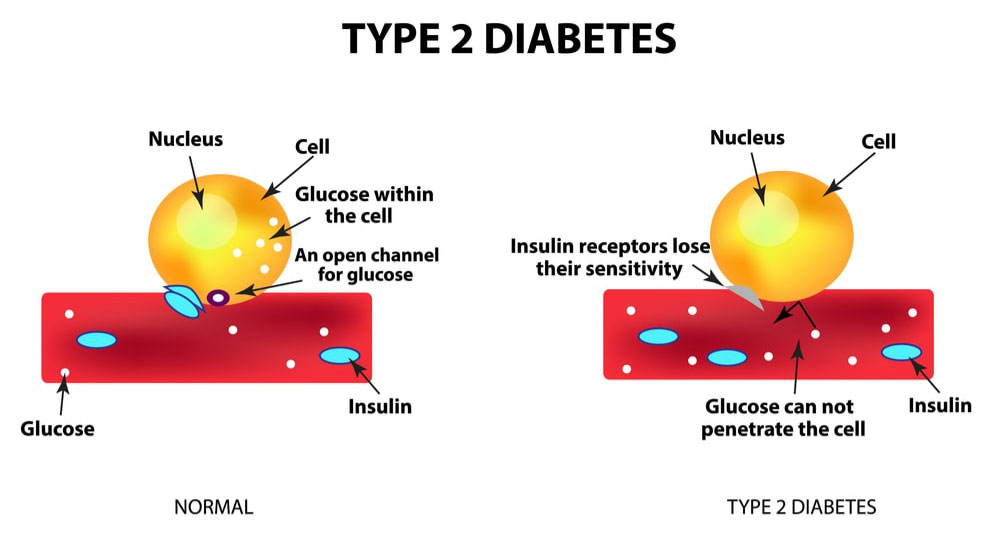
Diabetes Type 2 is often linked to obesity and concerns approximately 90% of diabetic patients26.
Finally, if you suffer from impaired glucose tolerance, then:
- just like in diabetes Type 2, your body is less sensitive to insulin,
- and your blood glucose levels are higher than normal but below those of a diabetes Type 2 patient.
Okay, it is now time to sharpen your mind to analyze the relationship between OSA and diabetes.
Studies have shown that:27 28 29
- If you have OSA, you are more likely to suffer from impaired glucose tolerance and diabetes Type 2.
- Respectively 50% and 30% of patients with OSA have impaired glucose tolerance and diabetes Type 2.
This is true independently of age and obesity.
Also, nondiabetic patients with OSA are at increased risk of developing:
- insulin resistance
- and diabetes.
Finally, most studies show that more than half of patients with Type 2 diabetes have some degree of OSA.30
Now, here is an interesting fact. A recent study of 131 patients diabetes Type 2, 70.2% of which had hypertension, showed that:
- Diabetes-related complications such as:
- retinopathy,
- neuropathy,
- nephropathy,
- or coronary artery disease,
were present in 55.5% of the patients.
- Those with moderate-to-severe OSA were 3.05 times were more likely to suffer from these.
This relationship was mediated by the presence of hypertension.31
But before we go on, here is an important piece of information for you….
…. The American Academy of Sleep Medicine (AASM) considers that the clinical evidence showing an increase in OSA amongst Type 2 diabetes patients is overwhelming.
As a result, they advise anyone with Type 2 diabetes (or hypertension for that matter) to be evaluated for sleep apnea by a board-certified sleep medicine physician.32
But why these associations between diabetes Type 2, glucose intolerance and OSA?
Frankly, the reasons are not well understood though some explanations could be:
- Because of sleep interruptions or intermittent sleep, OSA leads to a lack of oxygen (hypoxia) and poor rest.
- This can alter the way your body processes glucose and increases your risk of developing Type 2 diabetes.
Just like obesity is a risk factor for OSA, it is also a risk factor for diabetes. This could be part of the explanation.33
You may also be interested to read: can osa treatment help diabetes type patients or with abnormal glucose levels>
We touched upon hypertension, OSA and diabetes. It is now time to take a more in-depth look at how cardiovascular diseases are also associated with diabetes and OSA.
How are OSA, diabetes Type 2 and cardiovascular diseases related?
If you were to suffer from diabetes Type 2, the major potential causes of death would be?
If you thought cardiovascular diseases, you have the right answer.
They account for 50% of deaths amongst diabetic patients and lead to many types of disabilities34.
For instance, as a Type 2 diabetic patient, you would be twice more likely to have a heart attack or a stroke, than a healthy person.
Now, do you see the link with diabetes, cardiovascular diseases, and OSA?
OSA increases both the risks of:
- Cardiovascular diseases (hypertension, heart failure, stroke, coronary heart disease, and arrhythmias).
- Diabetes Type 2, which as we have just seen increases the risk of cardiovascular diseases.
Hence, if you suffer from sleep apnea, then you need treatment to prevent diabetes Type 2, and cardiovascular diseases, but….
…… even more so if you already suffer from diabetes Type 2 because you will be more at risk for cardiovascular diseases.
Unfortunately, the story does not end here. OSA is not only associated with increased risk for many diseases.
It is also associated with accidents.
And that is easy to understand right?
Sleepiness is a real threat to our safety when we drive.

Does OSA increase the chance of a motor vehicle accident?
Driver sleepiness contributes to almost 20% of all serious car crash injuries. And that is independent of alcohol consumption.35
These statistics speak for themselves, don’t you think?
And if in doubt … a study in Spain confirms these findings. It shows that with untreated OSA, you will be six times more likely to have a traffic accident.36
The cause is most probably drowsiness, and lack of concentration.
This was also suggested by another study. It showed that, if you are sleep deprived, your driving performance will be akin to driving after alcohol consumption.37
Finally, one last study showed that fall-asleep crashes and alcohol-related crashes were comparable in terms of fatalities and serious injuries.38
Are you curious to learn how many motor vehicle accidents could be avoided by treating OSA? Is so, then continue reading.
You will see that the numbers are astounding.
How many lives would be saved if apneic patients were treated with CPAP?
This information is available to us, thanks to a 2004 study.
They estimated:
- the number of OSA related collisions,
- their costs in human lives and dollars.
But they did not stop there.
They also estimated the human lives saved and monetary savings, by treating apneic patients with CPAP.
Here is a quick summary of the year 2000 data in the United States:
- 800,000 motor-vehicle collisions were OSA related.
- 1,400 human lives were lost with a cost of 15.9 billion dollars.
Treating apneic patients with CPAP would:39
- save 980 lives annually,
- cost about 3.18 billion dollars/year,
- but save 11.1 billion/year.
Now, OSA is also a cause of work-related accidents.
Curious to learn more?
If so, then jump over to the next section.
OSA and work-related accidents
OSA engenders daytime sleepiness.
You and I can easily infer that productivity at work will suffer.
Unfortunately, it does not stop there.
The injury rate or the chances of a work accident also increase.
By how much?
A review article, which analyzed 7 published studies, provides a useful answer. It concludes that “the odds of a work accident was found to be nearly double in workers with OSA.”
No wonder why the same authors strongly suggest that you should get screening for OSA in the workplace, in case your daily work is safety-sensitive.40
We talked about OSA and fragmented sleep.
But what about insomnia?
You may surmise that since OSA decreases the quality of your sleep, then there may be an association with insomnia.
If that is of interest to you, then stay with us and read on.
How are OSA and insomnia related?
According to sleep medicine dogma, insomnia is a sleeping disorder and so is OSA.
But did you know that the two often co-occur?
Research shows that 39%-58% of OSA patients also suffer from insomnia symptoms.
Likewise, 29%-67% of patients with insomnia also have OSA (apnea-hypopnea index > 5).41
Although cooccurrence does not imply a relationship of cause and effect, I am sure you are wondering about whether this link exists.
And if so, which comes first?
Does OSA cause insomnia or does insomnia cause OSA?
A 20 insomnia patients pilot study, run by Dr. Barry Krakow, sheds some light on this issue.
Patients’ selection excluded all those with signs or symptoms of sleep-disordered breathing (SDB).
The selection was based on physical traits or on patients’ answers to the .
Now, before the study, all patients identified their awakenings to:
- uncertain cause (50%),
- nightmares (45%),
- nocturia (35%),
- bedroom distractions (20%),
- or pain (15%).
None of them identified breathing symptoms as a cause of their waking up.
Reason why the results of the study were startling:
- To everybody’s surprise, 90% of awakenings were preceded by:
- sleep breathing events such as apnea,
- hypopnea,
- or respiratory effort-related event.
- 18 of the 20 patients woke up because of sleep-disorder breathing (SDB).
- Of these patients, 11 suffered from OSA since they had an average AHI of 14.4 (an AHI of 15 is a sign of moderate sleep apnea).42
Dr. Krakow explains, during an interview, that the number of insomniacs suffering from sleep breathing disorders is extremely high:43
- >90% for those complaining that their sleep aids do not work.
- Close to 100% for insomniacs with middle-of-the-night awakenings.
So, to conclude, if you are an insomniac who wakes up during the night then the cause may be OSA.
The good news is that OSA can be treated, and you stand an excellent chance of regaining a good quality sleep.
But OSA can influence the quality of your life in other ways… jump over to the next section to find out how.
OSA and erectile dysfunction (ED)
Not one, but several studies point to an important occurrence of ED among men suffering from OSA.
But how important is this occurrence?
The range is between 47,1% and 80%.
So, your partner’s snoring, or yours for that matter, may not be the only reason why OSA could influence your relation.
Also, the degree of severity of your OSA seems to play a role in the development of ED.
This seems to be associated with the importance of the decrease in blood oxygen levels. The frequency of apneas or hypopneas seems less important. 44
The exact mechanism, which could explain the association between OSA and ED, is unclear.
But studies have shown that testosterone drops with:45
- an increasing number of apneic events during sleep (increasing AHI),
- and decreasing oxygen levels in the blood.
We advise you to also read: can treating osa improve your erectile dysfunction>
Now, we are going to look at OSA and mood disorders.
How does OSA influence mood disorders?
Fatigue and depression may be associated with OSA.
And you know this is hugely important because depression is not just about feeling sad now and then.
Instead, the following symptoms may become pervasive, if you suffer from depression:
- a feeling of anxiety,
- loss of energy and pleasure for things you used to enjoy,
- difficulty in concentrating,
- sadness,
- hopelessness.

But how exactly is depression related to OSA?
Although the mechanism is not clear, disturbed sleep is probably one of the reasons.
If you have read this guide until now, you know that OSA leads to a poor-quality sleep.
Now, we all know how grumpy we can become after a night without proper sleep.
It is not difficult to accept that chronic inadequate sleep can wreak havoc in our capacity to cope with daily stress. This leads to lifelong mood problems.
Good solid sleep is critical to coping with the stress of modern living’s accelerated tempo.
In the presence of poor sleep caused by OSA, your brain will be less and less capable of managing stress.
Like any other organ, it will feel more and more exhausted. It will show symptoms of fatigue and depression during the day.
If in doubt about the influence of lack of sleep on mood, an 800 subjects study46 provides some useful information.
Whilst ensuring an equal balance between genders, it suggests a link between insomnia and depression.
It shows that people with insomnia have:
- greater depression levels by a factor of almost 10 than those whose sleep was normal,
- greater anxiety levels by a factor of 17, than people not having insomnia.
Now, insomnia symptoms include:
- struggling to fall asleep (onset insomnia),
- difficulty in staying asleep (maintenance insomnia),
- drowsiness during the day,
- and unrefreshing sleep.
The authors report that depression is highest among subjects who suffer from the first two symptoms at the same time.
So, if you only suffer from one (or a mixed form), you are less at risk.
By now you are probably thinking this is intriguing, but you may also be a little skeptical.
After all, is there any reliable data pointing to a link between depression and OSA?
Yes, there is data, thanks to a 18,980 subjects study.
Those with depression were found to be 5.26 more likely to also suffer from SDB. Now, OSA is the most common form of sleep-disordered breathing.47
Investigate further by reading also does treating obstructive sleep apnea decrease depressive symptoms>
Let’s now move on to a widespread disease – obesity – and see how that is associated with OSA.
How does obesity influence OSA?
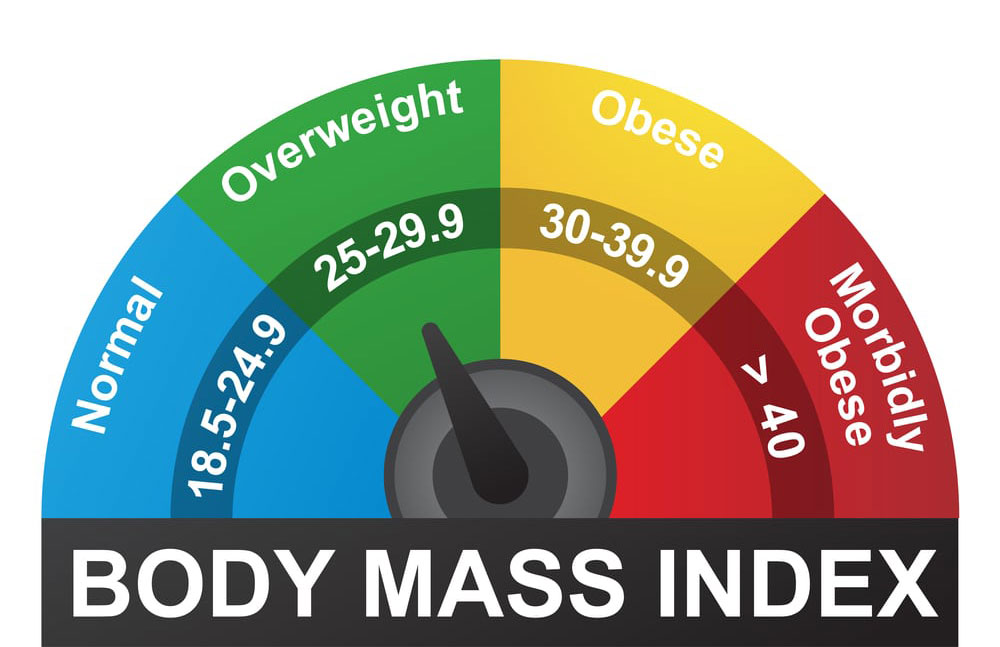
First things first. Before we look at the link between OSA and obesity, you need to know if you are obese or overweight.
To be classified as either one or the other, you need to weigh too much in relation to your height.
But how do you know how much is too much?
After listening to your spouse or partner’s pleas to lose some weight, do you want to know whether she or he is right? The Body Mass Index (BMI) can come to your rescue.
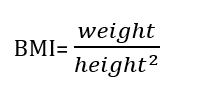
The BMI is quite simple to calculate
It is your weight (in kgs) divided by your height squared. So, the units are (kgs/m2).
You can use a simple smartphone’s app or surf the web to find a site that calculates it.
If you are an adult, then overweight is defined as IMC ≥ 25 Kg/m2 and obesity as IMC ≥ 30 Kg/m2.
Now, let’s investigate the relationship between obesity and OSA.
The former is indeed a significant risk factor for sleep apnea.
Why?
It has to do with fat accumulating around your neck and pharynx. It will narrow your superior airways (nose and throat) when you sleep.
So, if you are not obese, then you have total peace of mind?
Not so fast, because OSA is also observed in non-obese patients, for instance, those with enlarged tonsils.
But obesity remains an important risk factor for OSA.
Another explanation about why OSA and obesity are related is poor sleep quality.
There may even be a vicious circle between obesity, OSA and sleep deprivation.
How?
Let me explain.
Studies have shown that there may be a link between sleep deprivation and obesity. And we know that OSA causes sleep deprivation.48
This happens because disturbed sleep influences the hormonal mechanisms that regulate hunger and fullness.
Although further studies are required, poor quality or insufficient sleep may:
- Stop you from feeling full.
- Lower your daily energy expenditure by decreasing a hormone called leptin.
- Increase unnecessary food cravings (e.g., for sweet snacks) may result.
- Boost your appetite by increasing a hormone called ghrelin.
- Decrease your likelihood of exercising, because you will feel tired.
- Lead your body to secrete more insulin after a meal, which will increase sugar storage and thus your weight.
So, all this may lead to a vicious circle since:
- obesity affects OSA,
- which leads to fragmented sleep,
- and poor sleep may, in turn, affect obesity.
Before reading on, you may also want to check weight loss by bariatric surgery>
In the next section, we will analyze the link between OSA and cancer. This is the second leading cause of death globally.
How does OSA affect the risk of cancer?
For those used to read about OSA and its associated diseases, hearing about a potential link with cancer may come as a surprise.
As we have seen above, several studies have shown an association of OSA with:
- depression,
- hypertension,
- early death cardiovascular disease,
- …
but never with cancer.
That is, until Dr. F. Javier Nieto, an expert in sleep epidemiology, published an important paper (in 2012)49.
The publication is about sleep-disordered breathing and cancer mortality.
The lead author was less surprised than his readers by the findings, which showed:
- a 4.8 higher incidence of cancer deaths in patients with severe SDB (AHI ≥ 30) versus a healthy population,
- and 2.0 increased risk for moderate SDB (15 ≤ AHI ≤ 29.9),
in a 22-year mortality follow-up of 1,522 subjects chosen randomly from Wisconsin state employees.
The author’s reactions can be easily explained. Previous studies done in animals (and in vitro as well) had indicated that intermittent lack of oxygen promoted tumor growth.
It is still very early to say OSA causes cancer or contributes to its growth. More research is needed for this. Though the study is important because it shows a correlation for the first time.
Let’s now look at how OSA may affect your mental capacities such as:
- concentration,
- memory,
- and problem-solving.
How does OSA affect you’re your mental capabilities (cognitive functions)?
Even mental processes are affected!
We know how you feel: OSA seems to have pervasive health effects.
If you think about it though, OSA implies a fragmented sleep. So common sense tells us that it must impact our mental functioning somehow.
A review sheds some light on how OSA negatively impacts mental processes.50
OSA results in:
- attention/vigilance deficits;
- delayed long-term visual and verbal memory;
- disturbed visuospatial/constructional abilities such as:
- assembling different parts of an Ikea furniture,
- or building something with Lego,
- making a bed,
- buttoning a shirt,
- drawing, …;

Dog with strong mental capabilities - impaired executive function such as:
- gathering information,
- evaluating or changing behavior in response to the environment.
Language ability and movement during conscious mental activity (psychomotor functions) were instead found to be unaffected by OSA.
CPAP treatment of OSA appeared to improve:
- executive dysfunction,
- delayed long-term verbal and visual memory,
- attention/vigilance,
- and global conscious mental processes (cognitive functioning).
Another study supports the theory that disordered breathing accelerates memory loss.51
A study with a group of 2500 Alzheimer patients, aged between 55 and 90 years, showed interesting results. Memory declined 10 years earlier among those who had breathing problems such as snoring or sleep apnea.
How bad was the memory loss? Was it enough to prevent daily routine activities?
Albeit noticeable to their surroundings, fortunately, the loss was only mild.
It translated into forgetting recent events for instance.
Those who had been treated by CPAP instead behaved like those without breathing problems.
Their mental decline was as the same as the group non-affected by breathing disorders.
Also, Alzheimer development occurred 5 years earlier amongst untreated patients with breathing problems.
Lower oxygen is not the only factor that can explain these observations.
Lack of sleep could also cause an earlier onset of Alzheimer disease.
How?
By preventing the brain from eliminating toxins.
This is a process, which can only occur during deep sleep.
Since we talked about Alzheimer, let’s now look at its relationship with OSA.
How are OSA syndrome and Alzheimer disease related?
Did you know that Alzheimer and OSA show considerable overlap in the population?
What this means is that:
- if you suffer from one of the two,
- then you are more likely to also suffer from the other.
Although some suggest a link between the two, the mechanism is not understood.52
An article reviewing many published studies (meta-analysis) reports some interesting facts. It reveals a potential mechanism.53
Let’s analyze the facts.
The review shows that if you are a patient with Alzheimer disease, then you will be five times more likely …
Yes, you understood correctly,
… five times, more likely of presenting OSA than individuals of similar age with normal mental functions.
By mental functions we mean:
- memorization,
- processing thoughts,
- decision-making,
- learning,
The authors highlight that approximately half of the patients “have experienced OSA at some point after their initial diagnosis.”
They conclude by saying that if you are an Alzheimer patient, changes in:
- sleep quality and structure,
- cerebral blood flow,
- the presence of unstable molecules that damage cells (oxidative stress/free radicals),
may contribute to a decline in your mental functions worsening your disease.
Final Remarks
If you have found this article interesting, or if you want to learn more, then ….
… Do not stop here!
Instead, consider also the following readings:
- Obstructive Sleep Apnea: The Definitive Guide for 2020.
- (Chapter 1: Obstructive Sleep Apnea (OSA) and its Health Effects.)
- Chapter 2: Doctors Who Diagnose and Treat Obstructive Sleep Apnea.
- Chapter 3: Diagnosis of Obstructive Sleep Apnea (OSA).
- Chapter 4: Treating obstructive sleep apnea (OSA) with CPAP and dental appliances.
- Chapter 5: Treating Obstructive Sleep Apnea (OSA) with Surgery.
These are all in-depth articles of several thousand words, all based on the most recent scientific findings.
